- Courses
- GS Full Course 1 Year
- GS Full Course 2 Year
- GS Full Course 3 Year
- GS Full Course Till Selection
- Online Program
- GS Recorded Course
- NCERT (Recorded 500+ Hours)
- Polity Recorded Course
- Geography Recorded Course
- Economy Recorded Course
- AMAC Recorded Course
- Modern India, Post Independence & World History
- Environment Recoded Course
- Governance Recoded Course
- Science & Tech. Recoded Course
- International Relations and Internal Security Recorded Course
- Disaster Management Module Course
- Ethics Recoded Course
- Essay Recoded Course
- Current Affairs Recoded Course
- CSAT
- 5 LAYERED ARJUNA Mentorship
- Public Administration Optional
- ABOUT US
- OUR TOPPERS
- TEST SERIES
- FREE STUDY MATERIAL
- VIDEOS
- CONTACT US
Meghalaya Polio Case-Vaccine-Derived
Meghalaya Polio Case-Vaccine-Derived
On August 20, 2024, a case of vaccine-derived polio was confirmed in a two-year-old child from Tikrikilla, Meghalaya. This case is attributed to vaccine-derived poliovirus (VDPV), not wild poliovirus.
- India was declared polio-free by the World Health Organization (WHO) in 2014, following the last case of wild poliovirus in 2011.
Details of the Case:
- Location: Tikrikilla, West Garo Hills district, Meghalaya.
- Diagnosis: The child, displaying symptoms of poliomyelitis, was diagnosed with acute flaccid paralysis at a hospital in Assam’s Goalpara.
- Current Status:
- Samples: Stool and other samples from the child have been sent to testing centers in Kolkata and Mumbai.
- Response: Authorities are on high alert. The Meghalaya government is coordinating with relevant departments to address the situation.
What is Vaccine-Derived Polio?
- Definition: Vaccine-Derived Polio occurs when a strain of poliovirus originating from the oral polio vaccine (OPV) mutates and regains the ability to cause disease.
- Types of Poliovirus and Vaccines:
- Wild Poliovirus: The naturally occurring virus causing polio, with three types: Type 1, Type 2, and Type 3.
- Oral Polio Vaccine (OPV): Contains live, attenuated polioviruses. Effective in preventing polio and reducing transmission, but can mutate in rare cases.
- Inactivated Polio Vaccine (IPV): Contains killed polioviruses and is administered via injection. IPV does not cause vaccine-derived polio.
- How Vaccine-Derived Polio Occurs:
- Mutation: The weakened virus in OPV can mutate in the environment, potentially becoming pathogenic.
- Transmission: The mutated virus can spread in communities with low vaccination coverage, posing risks to those not fully immunized.
- Vaccine-Derived Poliovirus Types:
- VDPV Type 1
- VDPV Type 2
- VDPV Type 3
- Circulating Vaccine-Derived Poliovirus (cVDPV):
- Development: Rarely, the vaccine virus mutates into a form that causes paralysis.
- Global Context: Since 2000, over 10 billion doses of OPV have been administered globally, with 24 cVDPV outbreaks in 21 countries, resulting in fewer than 760 cases.
Prevention and Management:
- High Vaccination Coverage: Essential to minimize virus circulation and mutation risks.
- Switching to IPV: Some countries have replaced OPV with IPV to reduce vaccine-derived polio risks. IPV does not pose a risk of VDPV but requires high coverage to prevent outbreaks.
- Surveillance and Response: Robust systems monitor and detect polio cases and VDPV strains, with rapid response measures including vaccination campaigns and sanitation improvements.
Impact and Historical Context:
- Type 2 Eradication: OPV use has eradicated wild poliovirus Type 2. The phased withdrawal of Type 2-containing OPV addresses the persistent risk of VDPV Type 2.
- Global Efforts: Ongoing efforts focus on achieving high vaccination coverage and transitioning to safer vaccines for complete eradication.
Key Facts about Polio:
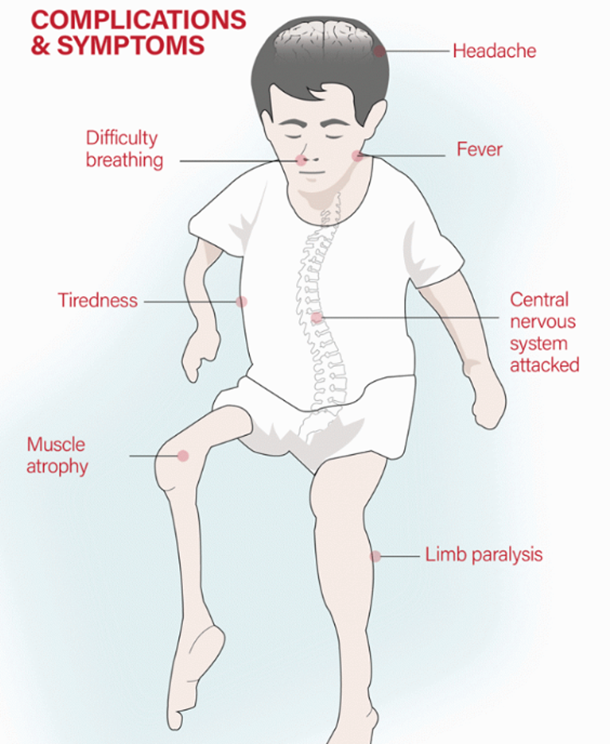
- Disease: A viral infection causing paralysis and potentially death by affecting the nervous system.
- Wild Poliovirus Strains: Type 1, Type 2, Type 3.
- Transmission: Primarily through the fecal-oral route, affecting the nervous system and primarily children under five.
- Vaccines Available:
- OPV: Administered as a birth dose, followed by three primary doses and a booster.
- IPV: Given alongside the third DPT vaccine under the Universal Immunization Programme (UIP).
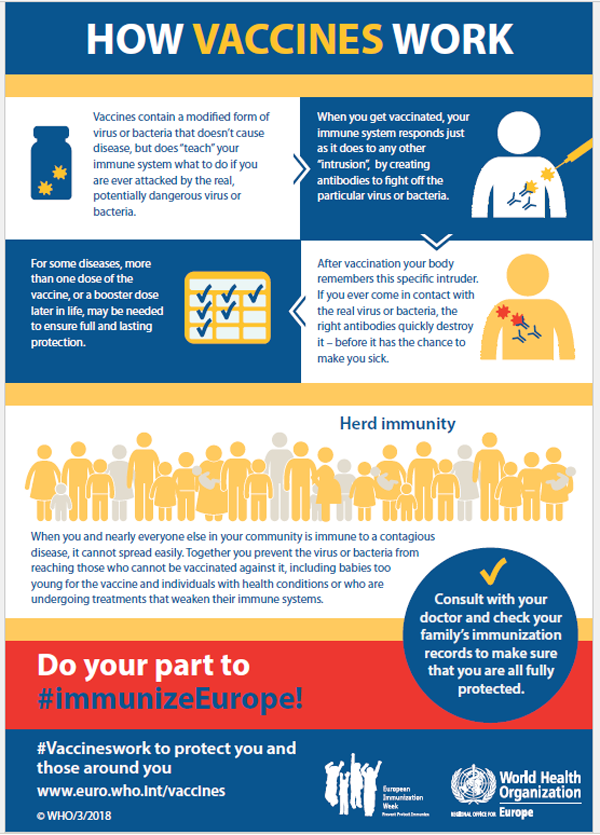
What is a Vaccine?Vaccines are crucial tools in preventing infectious diseases. They work by stimulating the body's immune system to recognize and fight specific pathogens, such as viruses or bacteria, without causing the disease itself. Here's a basic rundown:
|
Conclusion:
The recent detection of a vaccine-derived polio case in Meghalaya highlights ongoing challenges in global polio eradication. Despite India’s polio-free status regarding wild poliovirus, the risk of vaccine-derived strains persists, particularly in areas with low immunization coverage. Maintaining high vaccination rates, robust disease monitoring systems, and preparedness are crucial to preventing the spread of vaccine-derived poliovirus and safeguarding public health achievements. This case emphasizes the importance of sustaining effective immunization strategies and readiness in disease management.
Must Check: Best IAS Coaching In Delhi
UPSC Prelims Result 2024 Out: Expected Cut Off & Other Details, UPSC Prelims 2024 Answer with Explanation, Daily Prelims Quiz, Daily Current Affairs, MONTHLY CURRENT AFFAIRS TOTAL (CAT) MAGAZINE, Best IAS Coaching Institute in Karol Bagh, Best IAS Coaching Institute in Delhi, Daily Mains Question Answer Practice, ENSURE IAS UPSC Toppers, UPSC Toppers Marksheet, Previous Year Interview Questions, UPSC Syllabus